Program details
Subarachnoid Hemorrhage Treatment 【Kishiwada Tokushukai Hospital】
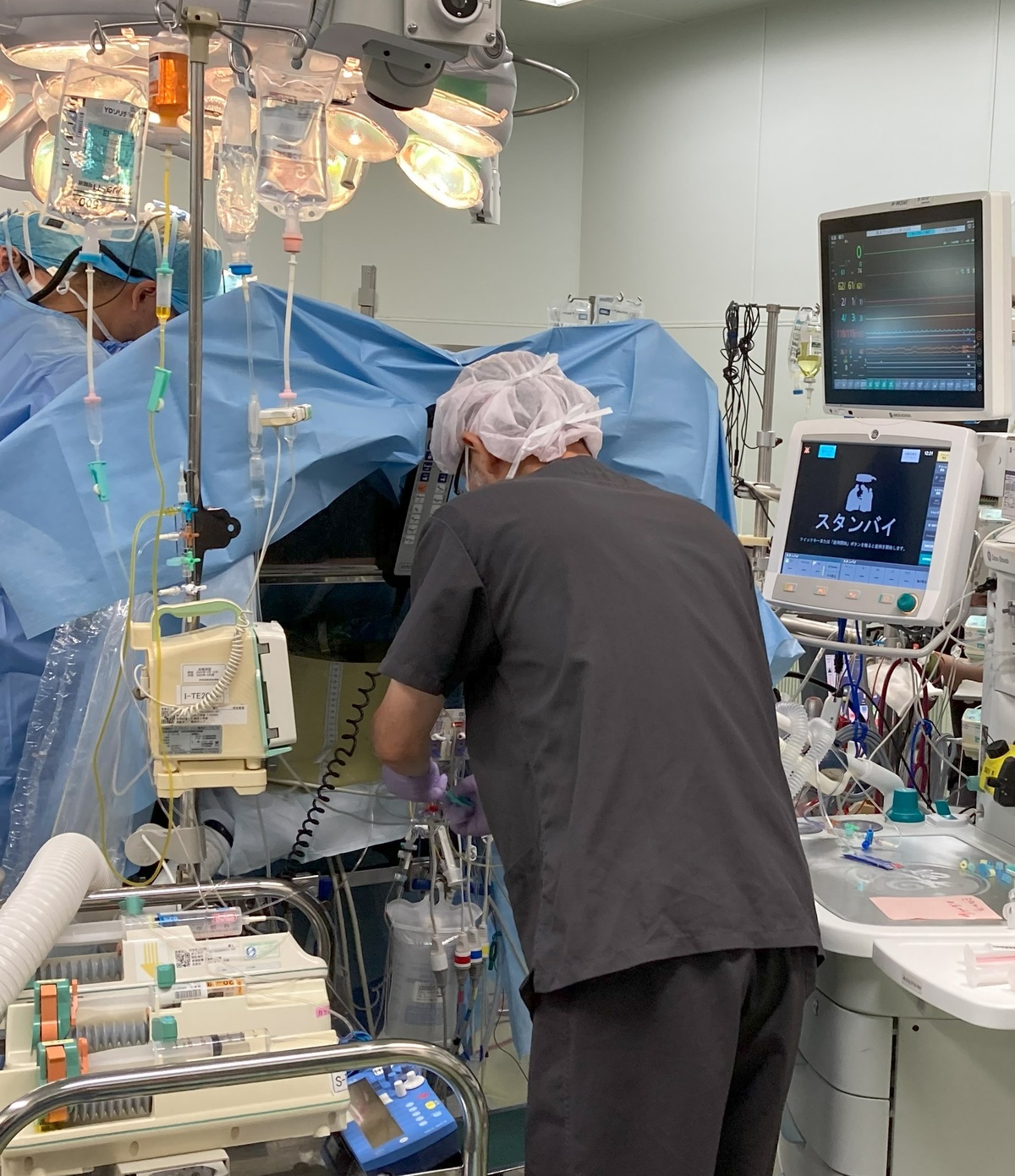
surgery
Kishiwada Tokushukai Hospital(Kinki/Osaka)
Prompt Response to Subarachnoid Hemorrhage
Reliable Treatment to Prevent Re-rupture
Subarachnoid hemorrhage is a life-threatening condition. To prevent re-rupture, early craniotomy or endovascular treatment is performed, along with thorough management to improve prognosis.
- Genres
-
- Department
- Disease
- Examination Items/Treatments/Surgical method
- Region/Organ
- Program Summary
- Subarachnoid Hemorrhage
- Be Aware of Sudden Severe Headache -
If you experience a sudden, severe headache unlike anything you've felt before, accompanied by nausea and vomiting, subarachnoid hemorrhage (SAH) should be suspected. SAH occurs when a blood vessel bulge (cerebral aneurysm) at the branch point of a brain artery ruptures. Blood leaking from the ruptured aneurysm fills the spaces in the brain, compressing the entire brain. Increased intracranial pressure poses a life-threatening risk.
SAH is classified into five grades of severity based on the condition at the time of onset. The mildest cases may involve only mild headache, which might lead patients to visit their primary care doctor and be mistakenly diagnosed with a common cold. Cases range from moderate, where patients are brought in with severe headache and vomiting, to the most severe cases, where patients present in a coma due to impaired consciousness. The more severe the condition upon hospital arrival, the poorer the prognosis.
While ruptured aneurysms may temporarily stop bleeding naturally, there is a high risk of re-rupture within hours to half a day. Each re-rupture exacerbates brain damage and quickly worsens the condition.
The treatment of SAH begins with preventing re-rupture of the ruptured aneurysm. Currently, there are two surgical methods for preventing re-rupture: craniotomy and endovascular treatment. Once the preventive surgery is successfully completed, intravenous therapy is needed to address vasospasm (cerebral vasospasm). Severe vasospasm can cause cerebral blood flow insufficiency, leading to cerebral infarction, which may result in paralysis or aphasia as aftereffects.
Furthermore, blood (hematoma) remaining in the brain spaces can obstruct cerebrospinal fluid (CSF) flow, leading to poor absorption and accumulation in the brain's ventricles (fluid-producing areas), causing ventricular enlargement—a condition called hydrocephalus. When acute hydrocephalus occurs, a rapid rise in intracranial pressure necessitates emergency ventricular drainage to remove CSF externally. For chronic hydrocephalus, a shunt surgery is performed to continuously redirect CSF within the body. There are two types of shunt procedures: ventriculoperitoneal shunt (draining CSF from the brain ventricles to the abdominal cavity) and lumboperitoneal shunt (draining CSF from the lumbar spinal space to the abdominal cavity), chosen based on the patient’s condition.
SAH triggers various events in the brain, requiring management of the ruptured aneurysm, treatment of cerebral vasospasm, and addressing hydrocephalus. Only after overcoming these challenges can patients be discharged in good health. However, the rate of social reintegration remains about 50%, with the remaining 50% either succumbing to the condition or suffering severe aftereffects, making SAH a highly feared disease.
- Medical Institutions
-
Kishiwada Tokushukai Hospital
〒596-0042
4-27-1 Kamoricho, Kishiwada City
- Examination Items
- Setup Date
- Excluded days
- Required Days/Hours
- Start/end time
- Eligibility Criteria/Exclusions for Treatment
- Eligibility Criteria
1. Medical Information:
- Diagnosis (e.g., subarachnoid hemorrhage, ruptured cerebral aneurysm)
- Detailed symptoms (e.g., severe headache, vomiting, impaired consciousness)
- Examination results from other hospitals (e.g., CT, MRI, angiography)
- Presence of comorbidities (e.g., hypertension, diabetes, kidney disease)
2. Treatment History:
- History of cerebrovascular treatments (e.g., craniotomy, catheter-based treatment)
- Current medications (e.g., anticoagulants, antiplatelet agents)
- Presence of allergies or adverse drug reactions
3. Age and Physical Strength:
- Assessment of whether elderly patients or those with comorbidities can tolerate surgery/treatment
- Evaluation of suitability for general anesthesia (including cardiopulmonary function)
4. Renal Function:
- Evaluation of renal function is required due to the use of contrast agents (caution if renal function is impaired)
5. Urgency:
- Determination of whether urgent intervention is required (e.g., acute subarachnoid hemorrhage, ruptured cerebral aneurysm)
6. Other Conditions:
- Ability to properly manage blood pressure and cooperate in pre- and postoperative blood pressure management
- Capability to manage antiplatelet or anticoagulant therapy
- Precautions / Contraindications
- 【Precautions and Contraindications】
1. Cases Excluded from Treatment:
- Severe renal dysfunction may make the use of contrast agents difficult, making catheter-based treatment contraindicated.
- Patients with poor blood pressure management require careful handling due to a higher risk of re-rupture.
- Patients unable to discontinue antiplatelet medications may face a high bleeding risk, which could limit treatment options.
2. Contraindications Related to General Anesthesia:
- In cases of impaired cardiopulmonary function or comorbidities that pose risks for general anesthesia, careful anesthetic management is required.
- For patients with drug allergies, medications must be reviewed in advance.
3. Risks of Treatment:
- Complications such as bleeding, thrombus formation, or cerebral infarction may occur during catheterization or surgery, with intracranial complications potentially having severe consequences.
- There is a postoperative risk of hydrocephalus or vasospasm, requiring continuous management.
---
【Important Pre-Procedure Information】
1. Preoperative Preparation:
- Follow the doctor's instructions regarding the discontinuation of anticoagulants or antiplatelet drugs.
- Undergo preoperative tests (e.g., CT, MRI, blood tests, renal function tests) to ensure diagnostic and therapeutic accuracy.
2. Postoperative Care and Risks:
- Be aware of risks such as bleeding, infection, or thrombus formation, and contact a medical institution immediately if abnormalities occur.
- Prepare for risks such as cerebral vasospasm and hydrocephalus with appropriate follow-up care after surgery.
3. Lifestyle and Rehabilitation:
- Avoid excessive exercise or activities that could lead to high blood pressure after discharge. Adopt lifestyle changes and engage in appropriate physical activity.
- Smoking cessation and proper dietary management are crucial for preventing arteriosclerosis and recurrence.
4. Hospitalization and Postoperative Schedule:
- Confirm the duration of hospitalization and rehabilitation period in advance.
- Attend regular follow-ups and check-ups after discharge.
5. Emergency Response:
- After discharge, immediately contact a medical institution if symptoms such as severe headache, vision impairment, nausea, or paralysis occur.
- Confirm the contact details of the responsible medical institution or physician for emergencies in advance.