Program details
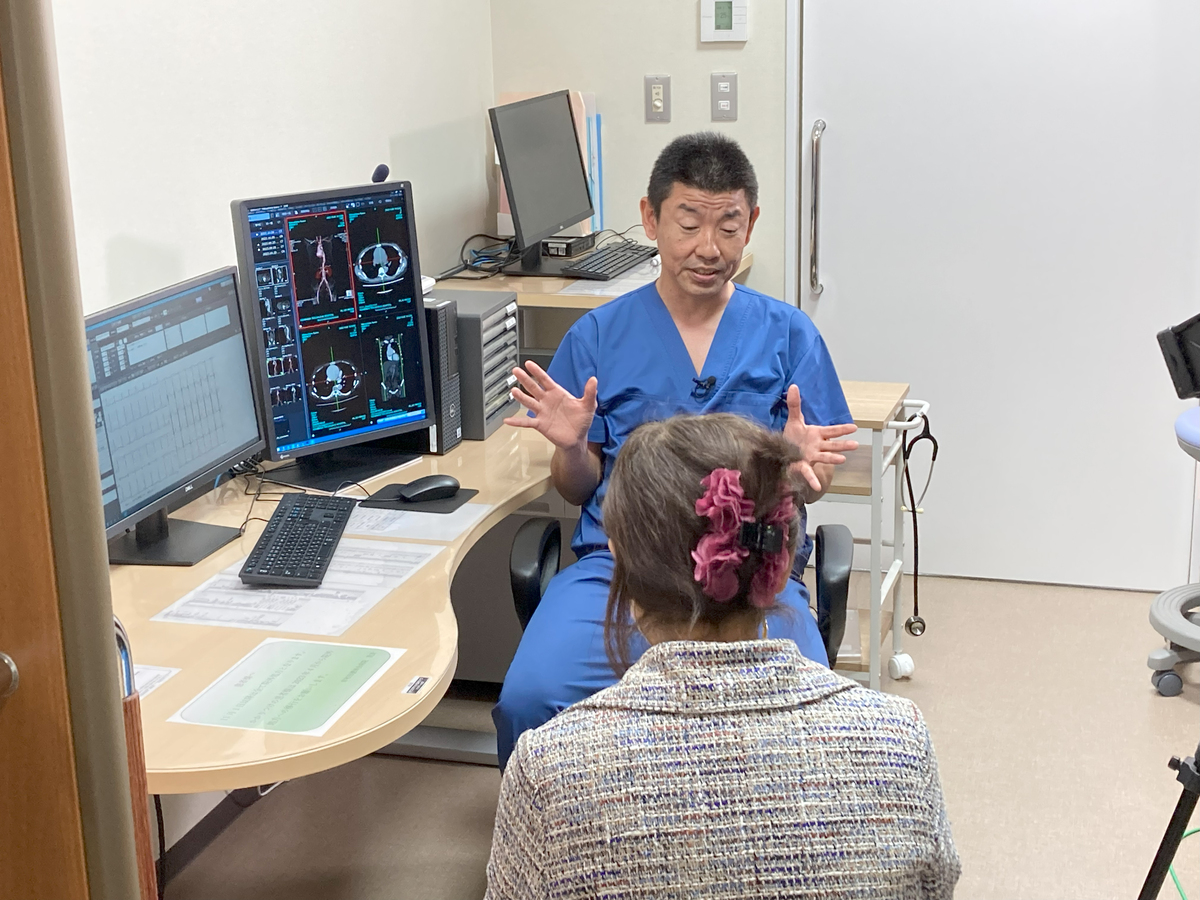
Peripheral Artery Disease - Arteriosclerosis Obliterans【Kishiwada Tokushukai Hospital】
surgery
Kishiwada Tokushukai Hospital(Kinki/Osaka)
Addressing Arteriosclerosis
Rapid Support with Emergency Treatment
We provide treatment through a combination of endovascular catheter therapy, surgical revascularization, and bypass surgery. For critical limb ischemia with ulcers, we offer comprehensive therapy, including bypass procedures for below-the-knee lesions and ulcer management.
- Genres
-
- Department
- Disease
- Examination Items/Treatments/Surgical method
- Region/Organ
- Program Summary
- Arteriosclerosis Obliterans
In collaboration with the Department of Cardiology, we provide treatment through a combination of endovascular catheter therapy, surgical revascularization, and bypass surgery. For critical limb ischemia with ulcers, we offer comprehensive therapy, including bypass procedures for below-the-knee lesions and ulcer management. A significant advantage of having the same team handle all treatments is the ability to assess cardiac and aortic conditions and develop a unified treatment plan.
Arterial Thrombosis
We provide 24/7 emergency surgical care. The incidence of cases with concurrent arteriosclerosis obliterans is increasing. With around-the-clock collaboration with the Department of Cardiology, we can deliver comprehensive treatment, including urgent bypass surgeries.
- Medical Institutions
-
Kishiwada Tokushukai Hospital
〒596-0042
4-27-1 Kamoricho, Kishiwada City
- Examination Items
- Setup Date
- Excluded days
- Required Days/Hours
- Start/end time
- Eligibility Criteria/Exclusions for Treatment
- [Eligibility Criteria]
1. Medical Information:
- Diagnosis (e.g., arteriosclerosis obliterans, arterial thrombosis, ischemic limb)
- Detailed symptoms (e.g., presence of ulcers, leg pain, numbness, cold sensation)
- Test results from other hospitals (e.g., vascular ultrasound, CT, angiography)
- Comorbidities (e.g., diabetes, chronic renal failure, hypertension)
2. Treatment History:
- History of vascular treatments (e.g., catheter-based therapy, bypass surgery)
- Current medications (e.g., anticoagulants, antiplatelet drugs)
- Assessment of side effects or effectiveness of previous treatments
3. Age and Physical Fitness:
- Evaluation of surgical tolerance in elderly patients or those with underlying conditions
- Assessment of overall health for suitability for catheter therapy or bypass surgery
4. Treatment Duration, Hospital Stay, and Time:
- Expected hospitalization period and postoperative rehabilitation duration
- Urgency of surgery and readiness for emergency procedures
5. Urgency:
- Determination of the need for emergency surgery in cases of acute thrombosis or critical limb ischemia
- Cases requiring 24/7 response readiness
6. Other Conditions:
- Eligibility for patients requiring long-term care for ulcers or critical limb ischemia
- Adjustment of treatment plans based on the patient’s lifestyle and preferences
- Precautions / Contraindications
- 1. Cases Excluded from Surgery:
- Severe comorbidities (e.g., advanced renal failure, liver failure, active infections) significantly increase surgical risks, making surgery inapplicable.
- Severely impaired cardiac function increases the risks of surgery and anesthesia, necessitating careful consideration of treatment options.
- Anatomical issues with blood vessels or valve conditions may make minimally invasive procedures (e.g., MICS or TAVI) unsuitable.
2. Contraindications for Specific Treatments:
- For **mechanical valves**, the need for lifelong anticoagulation (e.g., warfarin) may contraindicate use in patients at high risk of bleeding.
- In cases of infective endocarditis, surgery is contraindicated until the infection is controlled.
3. Considerations for Medication Therapy:
- Patients on anticoagulants or antiplatelet drugs may need to discontinue these before surgery, adhering strictly to the recommended discontinuation period.
- Special attention is required for patients with a history of allergies or adverse reactions to medications.
Preoperative Instructions to Communicate
1. Preoperative Preparation:
- All preoperative tests (e.g., echocardiography, CT, blood tests) must be completed as they are essential for accurate diagnosis and treatment planning.
- Adherence to instructions for discontinuation periods of anticoagulants or antiplatelet drugs is critical.
- Patients should follow any preoperative fasting or dietary restrictions.
2. Risks of Postoperative Complications:
- Risks such as bleeding, infection, or thrombosis must be explained. For mechanical valve procedures, lifelong anticoagulation therapy is mandatory, along with the associated bleeding risks.
- Patients should be informed about the potential for valve dysfunction or restenosis, emphasizing the importance of follow-up care.
3. Hospitalization and Postoperative Care:
- Post-surgery hospitalization typically lasts several days to a week, with close monitoring of recovery progress.
- Rehabilitation may be necessary, particularly to improve physical strength and support cardiac function.
- Adherence to post-discharge restrictions (e.g., activity limitations, dietary adjustments) is essential.
4. Regular Follow-Up:
- Regular outpatient visits and tests (e.g., echocardiography) are required post-surgery. For patients on anticoagulants, frequent blood tests will also be necessary.
- Immediate contact with a healthcare provider is crucial if any abnormal symptoms (e.g., chest pain, shortness of breath, fever) occur.
5. Cost Explanation:
- Provide an estimate of the costs for surgery, hospitalization, and follow-up care.
6. Emergency Response:
- Ensure patients have contact information for an emergency-ready medical facility in case of post-discharge issues such as chest pain, shortness of breath, or fever.